A sperm analysis report provides a comprehensive evaluation of semen and sperm parameters, crucial for assessing male fertility. It details factors like volume, sperm count, motility, and morphology, comparing them against WHO standards. Normal results are highlighted, guiding further fertility assessments.
1.1 Importance of Sperm Analysis
Sperm analysis is crucial for evaluating male fertility, providing insights into semen quality and sperm health. It helps diagnose infertility issues, assess treatment effectiveness, and guide lifestyle changes. By measuring parameters like volume, concentration, motility, and morphology, it identifies potential reproductive challenges. Accurate results enable healthcare providers to recommend appropriate interventions, ensuring informed decision-making for couples trying to conceive. Regular analysis also monitors sperm health over time, supporting overall reproductive well-being and fertility preservation efforts.
1.2 Purpose of a Sperm Analysis Report
A sperm analysis report serves as a diagnostic tool to assess male fertility by evaluating semen and sperm characteristics. It provides detailed insights into parameters like volume, concentration, motility, and morphology. The report helps identify potential reproductive issues, guiding fertility treatments and lifestyle adjustments. By comparing results to WHO standards, it offers a clear understanding of sperm health, enabling healthcare providers to make informed decisions and recommend appropriate interventions for individuals or couples seeking conception.

Semen Volume
Semen volume measures the amount of ejaculate, typically ranging from 1.5 to 5 mL. It plays a crucial role in sperm delivery and fertility potential.
2.1 Normal Range for Semen Volume
The normal semen volume typically ranges from 1.5 mL to 5 mL. This range ensures optimal sperm delivery and is crucial for fertility. WHO guidelines define 1.5 mL as the lower threshold for normal volume, with higher volumes generally associated with better sperm distribution and motility.
2.2 Factors Affecting Semen Volume
Semen volume can be influenced by various factors, including hormonal imbalances, infections, and lifestyle choices. Medical conditions like diabetes or prostate issues may reduce volume. Additionally, excessive alcohol consumption and smoking can negatively impact semen production, while stress and dehydration may also contribute to lower volumes. Proper sample collection and abstinence periods are crucial for accurate measurements.
Semen pH Levels
Semen pH levels are a critical component of sperm analysis reports, reflecting the biochemical environment of the semen. Normal pH ranges typically fall between 7.2 and 8.0, playing a vital role in sperm viability and overall reproductive health.
3.1 Normal Range for Semen pH
The normal pH range for semen is typically between 7.2 and 8.0. This slightly alkaline environment is essential for sperm survival and function. A pH outside this range may indicate underlying issues such as infections or blockages. Accurate measurement of semen pH is crucial for assessing male fertility and ensuring optimal conditions for sperm viability.
3.2 Implications of Abnormal Semen pH
An abnormal semen pH can indicate potential health issues. A pH below 7.2 may suggest infections or inflammation, while levels above 8.0 could indicate blockages or ejaculatory duct issues. Such imbalances can impair sperm function, reducing fertility. Identifying and addressing the cause is crucial for improving sperm health and overall reproductive well-being.
Sperm Concentration
Sperm concentration measures the number of sperm per milliliter of semen. A normal range is typically above 15 million/ml. Low concentration can affect fertility.
4.1 Normal Range for Sperm Concentration
The normal sperm concentration is typically defined as 15 million sperm per milliliter (ml) of semen or higher, according to the World Health Organization (WHO) guidelines. This parameter is crucial for assessing male fertility, as lower concentrations may indicate potential issues. Proper sample collection and abstinence periods are essential for accurate measurements. Maintaining this standard helps in evaluating the overall semen quality effectively.
4.2 Understanding Low Sperm Concentration
Low sperm concentration, or oligospermia, is diagnosed when sperm count falls below 15 million per milliliter. This condition can result from various factors, including hormonal imbalances, infections, or lifestyle choices. Identifying the underlying cause is essential for appropriate treatment. In cases of low concentration, further testing may be recommended to determine the best course of action for improving fertility and achieving conception.
Sperm Motility
Sperm motility refers to the ability of sperm to move efficiently, crucial for reaching and fertilizing the egg. It is categorized into progressive and non-progressive types, with progressive motility being more significant for successful conception. Proper motility is essential for fertility, and any deviations can impact reproductive success.
5;1 Normal Motility Levels
Normal sperm motility levels indicate that a sufficient percentage of sperm exhibit efficient movement. According to the World Health Organization (WHO), a normal semen analysis report typically shows that at least 40% of sperm have progressive motility. This means they move in a straight line with a strong, steady motion. Proper motility is crucial for successful fertilization, as it enables sperm to navigate through the female reproductive tract effectively.
5.2 Progressive vs. Non-Progressive Motility
Progressive motility refers to sperm moving in a straight line with a strong, steady motion, essential for reaching the egg. Non-progressive motility includes sperm moving in circles or with poor direction. A normal sperm analysis report typically shows a higher percentage of progressive motility, as this directly impacts fertility success. The WHO guidelines emphasize the importance of distinguishing between these categories to accurately assess sperm functionality and potential for successful fertilization.

Sperm Morphology
Sperm morphology evaluates the shape and structure of sperm, with normal forms typically exceeding 4% according to WHO standards. It assesses fertility potential by examining sperm for abnormalities.
6.1 Normal Morphology Levels
Normal sperm morphology levels are defined as having at least 4% of sperm with normal shapes according to WHO 5th Edition guidelines. This standard helps assess fertility potential, as higher percentages of normal forms correlate with better chances of conception. Abnormal morphology can indicate potential fertility issues, making this parameter critical in semen analysis reports for evaluating male reproductive health effectively.
6.2 Impact of Abnormal Morphology
Abnormal sperm morphology significantly impacts fertility, as irregularly shaped sperm often struggle to reach and fertilize an egg. Low normal form percentages (<4%) can reduce natural conception chances and may necessitate assisted reproductive techniques like IVF or ICSI. Early identification through semen analysis allows for timely medical or lifestyle interventions to address underlying issues and improve reproductive outcomes for individuals or couples trying to conceive.
WHO Guidelines for Sperm Analysis
WHO guidelines establish standardized parameters for sperm analysis, ensuring consistency in evaluating semen volume, sperm count, motility, and morphology. These benchmarks aid in accurate report interpretation and diagnosis.
7.1 Role in Setting Standards
The WHO guidelines play a crucial role in setting universal standards for sperm analysis. They provide reference values for semen volume, sperm count, motility, and morphology, ensuring consistency across laboratories. These standards are regularly updated based on scientific advancements, making them a reliable framework for clinicians and researchers. Adherence to WHO guidelines helps in accurate interpretation of semen analysis results, facilitating uniform diagnostic criteria globally.
7.2 Specific Parameters According to WHO
WHO guidelines specify normal ranges for semen parameters: volume should be ≥1.5 mL, pH between 7.2 and 8.0, sperm concentration ≥15 million/mL, and total sperm count ≥39 million/ejaculate. Motility requires ≥32% progressive and ≥40% total motile sperm. Morphology should have ≥4% normal forms. These parameters ensure standardized assessment of semen quality, aiding in accurate fertility evaluations and treatment decisions, and are widely adopted in clinical practice for consistent reporting and interpretation.

Sample Collection and Preparation
Proper semen collection involves masturbation after 2-7 days of abstinence, using a sterile container. The sample must be analyzed within 1 hour of collection to ensure accuracy.
8.1 Proper Collection Methods
Proper semen collection involves masturbation into a sterile container after 2-7 days of sexual abstinence. Avoid using lubricants or spermicides, as they can interfere with results. The sample should be collected in a private, comfortable setting to ensure completeness. Immediately label and deliver the container to the laboratory within 1 hour of collection to maintain sample integrity and accuracy in analysis.
8.2 Importance of Abstinence Period
An abstinence period of 2-7 days is recommended before semen collection to ensure accurate test results. This duration allows for optimal sperm concentration and motility, providing a reliable sample for analysis. Shorter or longer periods may lead to skewed results, affecting the evaluation of fertility parameters. Consistency in abstinence duration helps maintain uniformity in testing standards, ensuring reliable and comparable outcomes across different analyses.
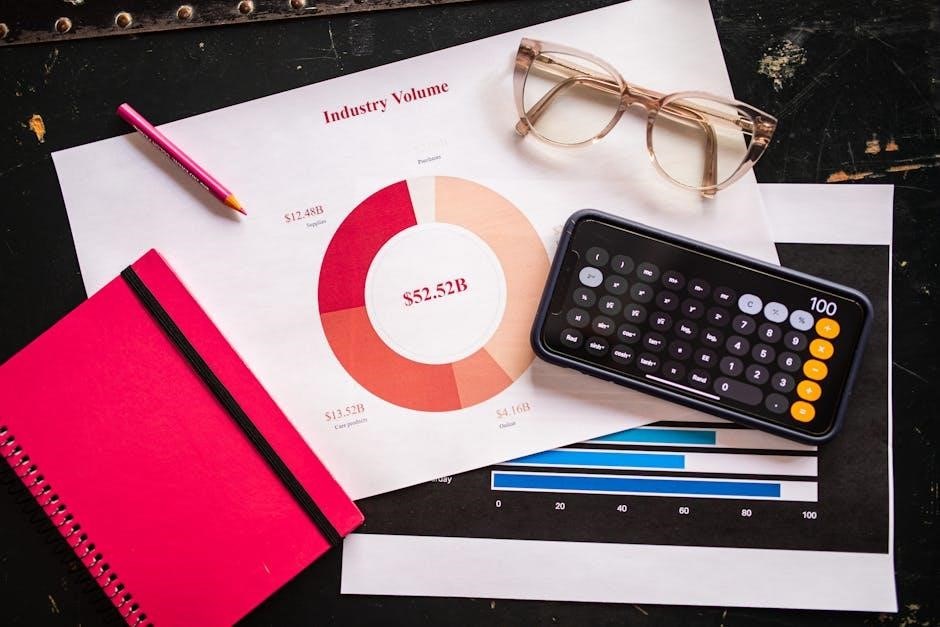
Interpreting the Report
Interpreting a sperm analysis report involves reviewing each section, from patient information to test results. Parameters are evaluated against WHO standards, with normal ranges clearly highlighted. Abnormal findings are noted, and clinical significance is explained, providing insights into fertility potential. The report includes comments and recommendations, guiding further actions based on the results.
9.1 Understanding the Results
Understanding the results of a sperm analysis report involves interpreting various parameters such as semen volume, sperm concentration, motility, and morphology. The report compares these values to WHO standards, highlighting normal ranges in green and abnormal results in amber. Detailed comments explain the clinical significance of each finding, ensuring clarity for both patients and healthcare providers. A guide is often included to help interpret the results effectively, making the report user-friendly and informative for fertility assessments.
9.2 Next Steps Based on Results
Based on the sperm analysis report, next steps are tailored to address any abnormalities. Normal results may require lifestyle adjustments, while low sperm count or motility could necessitate medical treatments like antibiotics or hormone therapy. In severe cases, assisted reproductive techniques such as IVF or ICSI are recommended. Follow-up testing is often advised to monitor progress and ensure the effectiveness of interventions, providing a clear path forward for fertility improvement and family planning.

Common Abnormalities and Implications
- Low sperm count can impair fertility and reduce conception chances.
- Poor motility may hinder sperm from reaching the egg.
- Abnormal morphology can signal genetic or health concerns.
10.1 Overview of Possible Issues
Common abnormalities in sperm analysis include low sperm count, poor motility, and abnormal morphology. These issues can indicate potential fertility challenges. Other factors like pH imbalances or low semen volume may also affect results. Identifying these abnormalities helps guide further testing or treatments to address underlying conditions. Understanding these issues is crucial for developing effective fertility management plans.